Address
1st floor B Wing Dinath Terrace Lady Jamshedji Road Landmark : Opposite City Light Theatre, , Mahim, Mumbai, Maharashtra 400016
Work Hours
Mon to Sat: 3PM - 7PM
Overview | Treatment | Surgery | Precautions | After Surgery Care

The urethra is a tube that carries urine from the bladder so it can be expelled from the body.
Usually, the urethra is wide enough for urine to flow freely through it. When the urethra narrows, it can restrict urinary flow. This is known as a urethral stricture.
Urethral stricture is a medical condition that mainly affects men.
Men are more likely to have a urethral disease or injury because of their longer urethra. For this reason, strictures are more common in men. They are rare in women and in infants.
Stricture (narrowing of the urethra) can happen at any point from the bladder to the tip of the penis. This narrowing restricts or slows the flow of urine. Some common causes are:trauma to the urethra
Rare causes include:
In most cases, no cause can be found.
In adults, urethral strictures are most often due to:
Posterior Urethral Stricture
Posterior urethral strictures happen in the first 1″ to 2″ of the urethra. This kind of stricture is due to an injury linked to a pelvic fracture (e.g., motor vehicle or industrial accident). In these cases, the urethra is disrupted, or completely cut and separated. Urine cannot pass. A catheter must be placed either through the abdomen into the bladder (suprapubic tube), or through the penis into the bladder. This lets urine drain until the stricture can be fixed.
Anterior Urethral Stricture
Anterior urethral strictures happen in the last 9″ to 10″ of the urethra. This kind of stricture is caused by:
Some men have an elevated risk of developing urethral stricture, especially those who have:
Urethral stricture can cause numerous symptoms, ranging from mild to severe. Some of the signs of a urethral stricture include:
A patient needs to undergo basic blood and urine tests apart from abdominal sonography. A urinalysis and a urine culture are done to rule out urinary infections. Tests may be done for Chlamydia, gonorrhea, and other sexually transmitted diseases. Urinary flow rates are measured. An X-ray (Ascending Urethrography) confirms the diagnosis, wherein contrast medium is injected into the urethral tube to outline the urethra and to define the extent of the stricture. Cystoscopy (telescopic inspection of the urethra and bladder) that is done during treatment will finally confirm the diagnosis.
The doctor will take a full medical history to help diagnose the underlying cause of urethral strictures.
They will ask about a person’s symptoms, when they started, and what makes them worse or better.
For males, a doctor will also conduct a physical exam to see whether there are any visible injuries or deformities to the penis. They may also recommend various testing methods to identify urethral problems. Tests include:
A doctor will use information from diagnostic studies to determine the severity of the urethral stricture and how it impacts surrounding structures.
There are many options depending on the size of the blockage and how much scar tissue is involved.
Treatments include:
There are no available drugs to help treat strictures.
Without treatment, you will continue to have problems with voiding. Urinary and/or testicular infections and stones could develop. Also, there is a risk of urinary retention (when you can’t pass urine), which could lead to an enlarged bladder and kidney problems.
This is usually performed in the urologist’s office with local anesthesia. The stricture is stretched using larger and larger dilators called “sounds.” A special balloon on a catheter can also stretch the tissue. But this stretching is not really a cure and needs to be repeated regularly. If the stricture comes back too quickly, you may be taught how to insert a catheter from time to time to prevent it from coming back. Side effects include bleeding and infection. Sometimes a “false passage” or second urethral channel may form from the stretching.
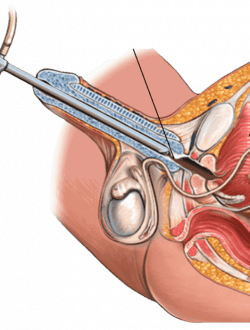
This uses a special scope that is moved along the urethra until the stricture is found.
A knife blade or laser at the end of the cystoscope is used to cut the stricture and create a gap. A catheter may be placed into the urethra to hold the gap open and let it heal. The suggested time to leave a catheter tube draining is based on the length of the stricture.
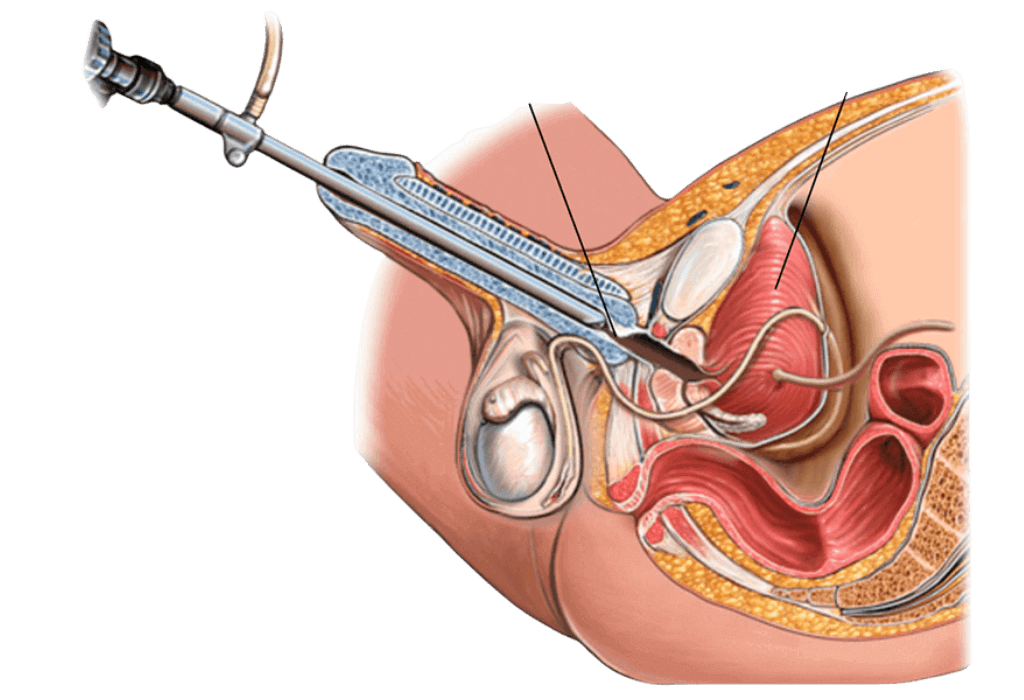
Many reconstructive procedures have been used to treat strictures, and some involve 1 or 2 operations. In all cases, the choice of repair is based on the location and length of the stricture and how serious it is. No single repair is right for all cases. The 2 main types are anastomotic urethroplasty and substitution urethroplasty.
Anastomotic Urethroplasty
This method is usually reserved for short urethral strictures. In this case, a cut is made between the scrotum and rectum. The urethra can then be reconnected after removing the stricture. This is usually performed as an outpatient procedure or with a short hospital stay. A small, soft catheter is left in the penis for 10 to 21 days. It is then removed after an X-ray is taken to make sure the repair has healed.
Substitution Urethroplasty
When the stricture is long, tissue can be transferred to replace the section that had the stricture. In difficult cases, substitution repairs may need to be done in stages. These repairs should be done by a urologist experienced with these surgeries. Overall the success rates are very good. The 3 kinds of substitution procedures are:
Free Graft
This method replaces or enlarges a section of the urethra using your own tissue. The tissue may be skin (taken from the shaft of the penis) or, more often, buccal mucosa (taken from inside the cheek). After surgery, you may need a short hospital stay and use a catheter for 2 or 3 weeks.
Skin Flap
With this surgery, flaps of skin are rotated from the penis to create the new section of the urethra. This is needed when a graft needs to be long, and the stricture is severe. These procedures are complex and should be done by a surgeon with plastic surgery experience. After surgery, you may need a short hospital stay and use a catheter for 2 or 3 weeks.
Staged
This method is used when local tissue will not work for a free graft or a skin flap.
First stage – The underside of the urethra is opened, which shows the full length of the stricture. A graft is secured to the opened urethra. The graft heals and matures for 3 months to a year. During that time, you will urinate through a new opening behind the stricture. This may mean that you have to sit down to urinate while the graft heals.
Second stage – Several months after the graft around the urethra has healed, and it is soft and flexible, the graft is formed into a tube. The urethra then returns to normal. A small, soft catheter is left in the penis for 10 to 21 days








Dr. Utture is Outstanding Doctor who gave good treatment to my 75 years old mother who was suffering from Kidney problem and stomach ache since last 3 years.
Thanks to Dr. Utture
Regards
I have been treated by Dr Anand Utture for multiple kidney stones.He is very knowledgeable, gives right advice, easily approachable and explains in simple language the problem and course of treatment.Takes special care of his patients, truly dedicated doctor
Extremely grateful to Dr Anand Utture for his timely and accurate diagnosis for treating my mother (81 years) for her kidney stones.
very experienced urologist & has done correct diagnosis & treatment of My Grandmother(81 yrs) for kidney stones.
















Most commonly, urethral strictures are managed by urologists, who are doctors with training and specialization in the urinary system.
Urethral stricture has a generally positive outcome. It is a treatable condition. However, this condition can happen again, requiring multiple procedures. Follow-up appointments with your healthcare professional will be needed after being treated for urethral stricture.
By avoiding injury to the pelvic area of the body, it may be possible to prevent some forms of urethral stricture. Taking care to avoid infection may also help prevent this condition.
These symptoms should get better in 1 or 2 days. You will probably be able to go back to most of your usual activities in 1 or 2 days. Drink extra water for the next few days. This care sheet gives you a general idea about how long it will take for you to recover. obstruction, you should drink plenty of water and limit your sodium (salt) intake.
If left untreated, a urethral stricture can cause serious problems, including bladder and kidney damage, infections caused by the obstruction of urine flow, and poor ejaculation and infertility in men. Fortunately, strictures can be successfully treated.
Dr Anand Utture is a Senior Urologist who is internationally recognized for his surgical expertise and academic contribution to the field of Urology.
Book AppointmentMake an appointment with your doctor if you have any signs and symptoms that worry you.
Seek immediate medical attention if you experience: