Address
1st floor B Wing Dinath Terrace Lady Jamshedji Road Landmark : Opposite City Light Theatre, , Mahim, Mumbai, Maharashtra 400016
Work Hours
Mon to Sat: 3PM - 7PM
Overview | Treatment | Surgery | Precautions | After Surgery Care
Testicular cancer is a growth of cells that starts in the testicles. The testicles, which are also called testes, are in the scrotum. The scrotum is a loose bag of skin underneath the penis. The testicles make sperm and the hormone testosterone.
Testicular cancer isn’t a common type of cancer. It can happen at any age, but it happens most often between the ages of 15 and 45.
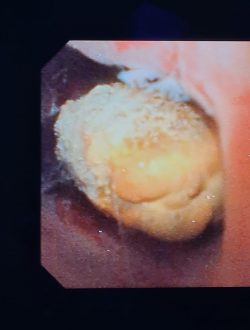
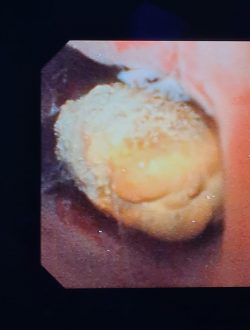
The first sign of testicular cancer often is a bump or lump on a testicle. The cancer cells can grow quickly. They often spread outside the testicle to other parts of the body.
Testicular cancer is highly treatable, even when it spreads to other parts of the body. Treatments depend on the type of testicular cancer that you have and how far it has spread. Common treatments include surgery and chemotherapy.
About 90% of all testicular cancer arises from germ cells in your testicles that clump together to form a mass or tumor. Germ cells eventually develop into sperm. Two types of testicular cancer arise from germ cells.
Some testicular cancer tumors consist of both seminoma and non-seminoma cells
A risk factor is anything that changes your chance of getting a disease such as cancer. Different cancers have different risk factors. Some risk factors, like smoking and diet, can be changed. Others, like a person’s age or family history, can’t be changed.
But having a risk factor, or even many does not mean that you will get the disease. Just as not having risk factors doesn’t mean you won’t get the disease. And some people who get the disease may not have had any known risk factors. Even if a person with testicular cancer has a risk factor, it’s often very hard to know how much that risk factor contributed to cancer.
Scientists have found few risk factors that make someone more likely to develop testicular cancer. Most boys and men with testicular cancer don’t have any of the known risk factors. Risk factors for testicular cancer include:
.
One of the main risk factors for testicular cancer is a condition called cryptorchidism, or undescended testicle(s). This means that one or both testicles fail to move from the abdomen (belly) into the scrotum before birth. Males with cryptorchidism are many times more likely to get testicular cancer than those with normally descended testicles. Normally, the testicles develop inside the abdomen of the fetus and they go down (descend) into the scrotum before birth. But in about 3% of boys, the testicles do not make it all the way down before the child is born. Sometimes one or both testicles stay in the abdomen. In other cases, the testicles start to descend but stay in the groin area. Most of the time, undescended testicles continue moving down into the scrotum during the child’s first year of life. If the testicle hasn't descended by the time a child is a year old, it probably isn’t going to do it on its own. Sometimes a surgical procedure known as orchiopexy is needed to move the testicle down into the scrotum. The risk of testicular cancer might be a little higher for men whose testicle stayed in the abdomen as opposed to one that has descended at least partway. If cancer does develop, it's usually in the undescended testicle, but about 1 out of 4 cases occur in the normally descended testicle. Because of this, some doctors conclude that cryptorchidism doesn’t actually cause testicular cancer, but that there's something else that leads to both testicular cancer and abnormal positioning of one or both testicles.
Having a father or brother with testicular cancer increases the risk that you will get it, too. But only a small number of testicular cancers occur in families. Most men with testicular cancer do not have a family history of the disease. Klinefelter's syndrome is an inherited disease that's also linked to an increased risk of testicular cancer.
Some evidence has shown that men infected with the human immunodeficiency virus (HIV), particularly those with AIDS, are at increased risk. No other infections have been shown to increase testicular cancer risk.
A personal history of testicular cancer is another risk factor. About 3% or 4% of men who have been cured of cancer in one testicle will at some point develop cancer in the other testicle.
About half of testicular cancers occur in men between the ages of 20 and 34. But this cancer can affect males of any age, including infants and elderly men
The risk of testicular cancer among white men is about 4 to 5 times that of Black and Asian-American men. The risk for American Indians falls between that of Asians and whites. The reason for these differences is not known. Worldwide, the risk of developing this disease is highest among men living in the United States and Europe and lowest among men living in Africa or Asia.
Several studies have found that tall men have a somewhat higher risk of testicular cancer, but some other studies have not. Most studies have not found a link between testicular cancer and body weight.
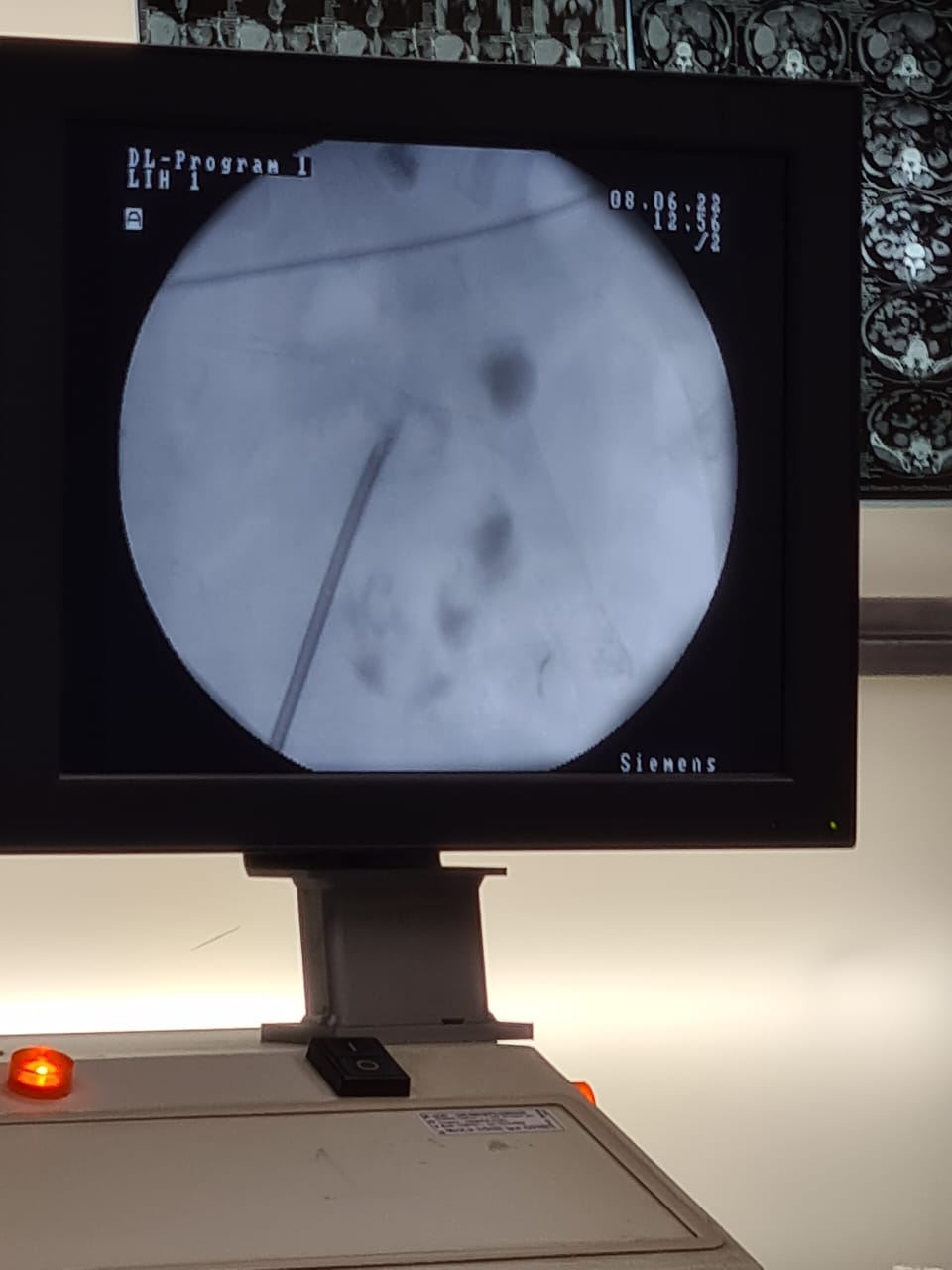
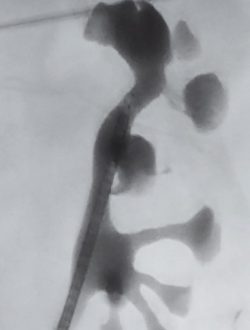
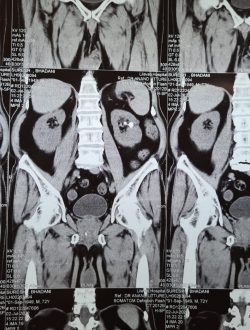
If your urologist finds cancer through these exams, he or she will want to learn the exact cancer cell-type and if it has spread. This is called “staging.” This process helps the doctor learn which treatments are best.
Unlike other cancers, your doctor does not take a tissue sample (biopsy) before surgery. With testicular cancer, cells are looked at after surgery is done to remove the cancerous tissue.”
Usually, testicular cancer only happens in one testicle. Signs and symptoms of testicular cancer include:
A lump or swelling in either testicle
A feeling of heaviness in the scrotum
A dull ache in the lower belly or groin and Back pain
Sudden swelling in the scrotum
Pain or discomfort in a testicle or the scrotum
Enlargement or tenderness of the breast tissue
You might find lumps, swelling or other symptoms of testicular cancer on your own. They can be detected during an exam by a health care provider too. You’ll need other tests to see if testicular cancer is causing your symptoms.
Tests used to diagnose testicular cancer include:
Ultrasound. A testicular ultrasound test uses sound waves to make pictures. It can be used to make pictures of the scrotum and testicles. During an ultrasound, you lie on your back with your legs spread. A healthcare provider puts a clear gel on the scrotum. A hand-held probe is moved over the scrotum to make the pictures.
Ultrasound gives your provider more clues about any lumps around the testicle. It can help your provider see whether the lumps look like something that isn’t cancer or if they look like cancer. An ultrasound shows whether the lumps are inside or outside the testicle. Lumps inside the testicle are more likely to be testicular cancer.
Blood tests. A blood test can detect proteins made by testicular cancer cells. This type of test is called a tumor marker test. Tumor markers for testicular cancer include beta-human chorionic gonadotropin, alpha-fetoprotein and lactate dehydrogenase. Having these substances in your blood doesn’t mean you have cancer. Having levels higher than is typical is a clue your health care team uses to understand what’s going on in your body.
Surgery to remove a testicle. If your health care provider thinks a lump on your testicle may be cancerous, you might have surgery to remove the testicle. The testicle is sent to a lab for testing. The tests can show whether it’s cancerous.
Testicular cancer surgery carries a risk of bleeding and infection. If you have surgery to remove lymph nodes, there’s also a risk that a nerve might be cut. Surgeons take great care to protect the nerves. Sometimes cutting a nerve can’t be avoided. This can lead to problems with ejaculating, but it generally doesn’t affect your ability to get an erection. Ask your health care provider about options for preserving your sperm before surgery.
Chemotherapy
Chemotherapy treatment uses strong medicines to kill cancer cells. Chemotherapy travels throughout the body. It can kill cancer cells that may have spread beyond the testicle.
Chemotherapy is often used after surgery. It can help kill any cancer cells that are still in the body. When testicular cancer is very advanced, sometimes chemotherapy is used before surgery.
Side effects of chemotherapy depend on the specific medicines being used. Common side effects include fatigue, hearing loss and an increased risk of infection.
Chemotherapy also may cause your body to stop making sperm. Often, sperm production starts again as you get better after cancer treatment. But sometimes losing sperm production is permanent. Ask your healthcare provider about your options for preserving your sperm before chemotherapy.
Radiation therapy
Radiation therapy uses high-powered energy beams to kill cancer cells. The radiation can come from X-rays, protons, and other sources. During radiation therapy, you’re positioned on a table and a large machine moves around you. The machine points the energy beams at precise points on your body.
Radiation therapy is sometimes used to treat the seminoma type of testicular cancer. Radiation therapy may be recommended after surgery to remove your testicle.
Radiation therapy typically isn’t used to treat the nonseminoma type of testicular cancer.
Side effects may include nausea and fatigue. Radiation therapy also can temporarily lower sperm counts. This can affect your fertility. Ask your healthcare provider about your options for preserving your sperm before radiation therapy.
Immunotherapy
Immunotherapy is treatment with a medicine that helps your body’s immune system kill cancer cells. Your immune system fights off diseases by attacking germs and other cells that shouldn’t be in your body. Cancer cells survive by hiding from the immune system. Immunotherapy helps the immune system cells find and kill cancer cells.
Immunotherapy is sometimes used for advanced testicular cancer. It might be an option if cancer doesn’t respond to other treatments.
If you feel a lump or notice any change, talk to your doctor immediately. Cases of testicular cancer that are detected early on have a 99% survival rate.
Some testicular cancer treatments can leave you infertile.
When the cancerous testicle is surgically removed, the remaining testicle is still capable of producing enough sperm to father a child.
If fatherhood is on your mind, it’s important to take steps that will increase your odds of becoming a father before beginning treatments. Storing sperm in a sperm bank for later use is a very common option.
It is safe to have sex after your body recovers from a testicular cancer treatment.
Each case is different, but you can expect to return to a normal sex life after just a few months.











Dr. Utture is Outstanding Doctor who gave good treatment to my 75 years old mother who was suffering from Kidney problem and stomach ache since last 3 years.
Thanks to Dr. Utture
Regards
I have been treated by Dr Anand Utture for multiple kidney stones.He is very knowledgeable, gives right advice, easily approachable and explains in simple language the problem and course of treatment.Takes special care of his patients, truly dedicated doctor
Extremely grateful to Dr Anand Utture for his timely and accurate diagnosis for treating my mother (81 years) for her kidney stones.
very experienced urologist & has done correct diagnosis & treatment of My Grandmother(81 yrs) for kidney stones.
















Testicular cancer largely affects younger men, particularly those between the ages of 20 and 40. The average age of a testicular cancer patient is 33 years old. While testicular cancer is not a commonly diagnosed disease—one in every 250 men will be diagnosed during their lifetime—it is one of the most prevalent cancers for younger men. It rarely affects boys under the age of 20 (an estimated 6% of cases) or men over the age of 55 (an estimated 8% of cases). Testicular cancer is highly responsive to treatment, with survival rates as high as 99%, even if diagnosed at a later stage. Treatment for testicular cancer can include a combination of surgery, radiation therapy, chemotherapy and clinical trials.
Testicular cancer often develops in just one of the testicles, meaning that the other testicle can continue to generate testosterone and function as normal. If surgery is used to remove the affected testicle, many men are able to maintain fertility with the healthy testicle. However, if both testicles are affected and need to be removed, the patient will not maintain fertility. Additionally, testicular cancer itself may reduce fertility, even if one testicle is unaffected.
Chemotherapy and radiation therapy can also affect fertility. Chemotherapy for testicular cancer often causes infertility on a temporary basis. After some time has passed from the end of chemotherapy, fertility returns for many men. However, it is possible that fertility will not return, even after treatment has ended.
When radiation therapy is used to treat testicular cancer, the unaffected testicle will be shielded to help protect it from the high-energy waves used in this treatment. As long as the healthy testicle is not damaged by the radiation therapy, fertility will be maintained. However, even with the shield, there is a risk of losing fertility in the healthy testicle. Additionally, your physician may recommend waiting for a period of time after receiving this treatment before trying to have a child.
Because chemotherapy can’t distinguish between rapidly dividing cancer cells and healthy cells in the body that also divide rapidly, it can destroy those healthy cells along with the cancer cells and cause side effects for patients. Side effects vary from patient to patient based on factors like the type of medications used, the dosage and the length of treatment.
Possible side effects of chemotherapy for testicular cancer treatment include:
Certain chemo medications can cause additional side effects, as well. These might include shortness of breath, hearing loss, neuropathy (nerve damage) and kidney damage. Again, this depends on the type of medication used, and medical oncologists can take measures to prevent or reduce these side effects.
The side effects of chemotherapy are typically short-term and go away after treatment is concluded; however, sometimes they can last longer.
The prognosis for testicular cancer is excellent. This form of cancer is treated successfully in more than 95% of cases. Even people with unfavorable risk factors have, on average, a 50% chance of being cured.
Dr Anand Utture is a Senior Urologist who is internationally recognized for his surgical expertise and academic contribution to the field of Urology.
Book AppointmentMake an appointment with your doctor if you have any signs and symptoms that worry you.
Seek immediate medical attention if you experience: