Address
1st floor B Wing Dinath Terrace Lady Jamshedji Road Landmark : Opposite City Light Theatre, , Mahim, Mumbai, Maharashtra 400016
Work Hours
Mon to Sat: 3PM - 7PM
Overview | Treatment | Surgery | Precautions | After Surgery Care

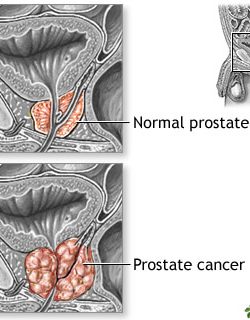
Prostate cancer is cancer that occurs in the prostate. The prostate is a small walnut-shaped gland in males that produces the seminal fluid that nourishes and transports sperm.
Prostate cancer is one of the most common types of cancer. Many prostate cancers grow slowly and are confined to the prostate gland, where they may not cause serious harm. However, while some types of prostate cancer grow slowly and may need minimal or even no treatment, other types are aggressive and can spread quickly.
Prostate cancer that’s detected early — when it’s still confined to the prostate gland — has the best chance for successful treatment.
Almost all prostate cancers are adenocarcinomas. These cancers develop from the gland cells (the cells that make the prostate fluid that is added to the semen).
Other types of cancer that can start in the prostate include:
These other types of prostate cancer are rare. If you are told you have prostate cancer, it is almost certain to be an adenocarcinoma.
Some prostate cancers grow and spread quickly, but most grow slowly. In fact, autopsy studies show that many older men (and even some younger men) who died of other causes also had prostate cancer that never affected them during their lives. In many cases, neither they nor their doctors even knew they had it.
About 1 man in 8 will be diagnosed with prostate cancer during his lifetime.
Prostate cancer is more likely to develop in older men and in non-Hispanic Black men. About 6 cases in 10 are diagnosed in men who are 65 or older, and it is rare in men under 40. The average age of men at diagnosis is about 66.
As men age, their risk of getting prostate cancer goes up. It is rarely found in men younger than age 40. Damage to the genetic material (DNA) of prostate cells is more likely for men over the age of 55. Damaged or abnormal prostate cells can begin to grow out of control and form tumors. Age is a well-known risk factor for prostate cancer. But, smoking and being overweight are more closely linked with dying from prostate cancer.
African American men have, by far, the highest incidence of the disease. One in six African American men will get prostate cancer. African American men are more likely to get prostate cancer at an earlier age. They are also more like to have aggressive tumors that grow quickly, spread and cause death. The reason why prostate cancer is more prevalent in African American men is unclear yet it may be due to socioeconomic, environmental, diet or other factors. Other ethnicities, such as Hispanic and Asian men, are less likely to get prostate cancer.
Men with a family history of prostate cancer also face a higher risk of also developing the disease. A man is 2 to 3 times more likely to get prostate cancer if his father, brother or son had it. This risk increases with the number of relatives diagnosed with prostate cancer. The age when a close relative was diagnosed is also an important factor.
Studies show prostate cancer risk may double for heavy smokers. Smoking is also linked to a higher risk of dying from prostate cancer. However, within 10 years of quitting, your risk for prostate cancer goes down to that of a non-smoker the same age
Prostate cancer numbers and deaths vary around the world but are higher in North America and Northern Europe. Higher rates may be due to better or more screening procedures, heredity, poor diets, lack of exercise habits, and environmental exposures.
Diet and lifestyle may affect the risk of prostate cancer. It isn't clear exactly how. Your risk may be higher if you eat more calories, animal fats, refined sugar and not enough fruits and vegetables. A lack of exercise is also linked to poor outcomes. Obesity (or being very overweight) is known to increase a man's risk of dying from prostate cancer. One way to decrease your risk is to lose weight, and keep it off.
About 1 in 9 men will receive a prostate cancer diagnosis during their lifetime. Prostate cancer is second only to skin cancer as the most common cancer affecting males. There are many successful treatments — and some men don’t need treatment at all. Still, approximately 33,000 men die from the disease every year.
Men over the age of 55 are more prone to the disease. Your chances of developing prostate cancer increase as you age. In fact, 60% of prostate cancers occur in men over the age of 65. Other risk factors include:
Different people have different symptoms for prostate cancer. Some men do not have symptoms at all.If you have any of the following symptoms, be sure to see your doctor right away—
Blood in the urine or semen
Difficulty starting urination
Weak or interrupted flow of urine
Urinating often, especially at night
Trouble emptying the bladder completely
Pain or burning during urination
Pain in the back, hips, or pelvis that doesn’t go away
Fatigue
Painful ejaculation
Keep in mind that these symptoms may be caused by conditions other than prostate cancer.
Your doctor may consider these factors when choosing a diagnostic test:
Screening means testing for a disease even if you have no symptoms. The prostate specific antigen (PSA) blood test and digital rectal examination (DRE) are two tests that are used to screen for prostate cancer. Both are used to detect cancer early. However, these tests are not perfect. Abnormal results with either test may be due to benign prostatic enlargement (BPH) or infection, rather than cancer.
The American Urological Association (AUA) recommends talking with your healthcare provider about whether or not you should be screened. To find out if prostate cancer screening is a good idea, use our Prostate Cancer Screening Assessment Tool. Share your results with your healthcare provider when you talk about the benefits and risks of screening.
The two main types of screenings are:
The prostate-specific antigen (PSA) blood test is one way to screen for prostate cancer. This blood test measures the level of PSA in the blood. PSA is a protein made only by the prostate and prostate cancers. The test can be done in a lab, hospital or healthcare provider’s office.
Very little PSA is found in the blood of a man with a healthy prostate. A low PSA is a sign of prostate health. A rapid rise in PSA may be a sign that something is wrong. Prostate cancer is the most serious cause of a high PSA result. Another reason for a high PSA can be benign (non-cancer) enlargement of the prostate. Prostatitis, inflammation of the prostate, can also cause high PSA results.
In cancer care, different types of doctors—including medical oncologists, surgeons, and radiation oncologists, urologist, physician —often work together to create an overall treatment plan that may combine different types of treatments to treat the cancer. This is called a multidisciplinary team. Cancer care teams include a variety of other health care professionals, such as palliative care experts, physician assistants, nurse practitioners, oncology nurses, social workers, pharmacists, counselors, dietitians, physical therapists, and others
Surgery involves the removal of the prostate and some surrounding lymph nodes during an operation. A surgical oncologist is a doctor who specializes in treating cancer using surgery. For prostate cancer, a urologist or urologic oncologist is the surgical oncologist involved in treatment. The type of surgery depends on the stage of the disease, the patient’s overall health, and other factors.
Radical (open) prostatectomy. A radical prostatectomy is the surgical removal of the entire prostate and the seminal vesicles. Lymph nodes in the pelvic area may also be removed. This operation has the risk of affecting sexual function. Nerve-sparing surgery, when possible, increases the chance that the patient can maintain sexual function after surgery by avoiding surgical damage to the nerves that allow erections and orgasm to occur. Orgasm can occur even if some nerves are cut because these are separate processes. Urinary incontinence is also a possible side effect of radical prostatectomy. To help resume normal sexual function, drugs, penile implants, or injections may be recommended. Sometimes, another surgery can fix urinary incontinence.
Robotic or laparoscopic prostatectomy. This type of surgery is less invasive than a radical prostatectomy and may shorten recovery time. A camera and instruments are inserted through small keyhole incisions in the patient’s abdomen. The surgeon then directs the robotic instruments to remove the prostate gland. In general, robotic prostatectomy causes less bleeding and less pain, but the sexual and urinary side effects are similar to those of a radical (open) prostatectomy. Talk with your doctor about whether your treatment center offers this procedure and how it compares with the results of the radical (open) prostatectomy.
Bilateral orchiectomy. Bilateral orchiectomy is the surgical removal of both testicles. It is described in detail in “Systemic treatments” below.
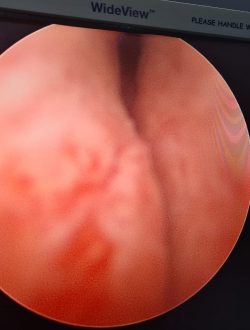
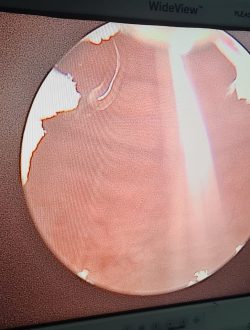
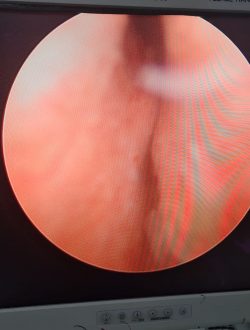
Transurethral resection of the prostate (TURP). TURP is most often used to relieve symptoms of a urinary blockage, not to treat prostate cancer. In this procedure, with the patient under full anesthesia, which is medication to block the awareness of pain, a surgeon inserts a narrow tube with a cutting device called a cystoscope into the urethra and then into the prostate to remove prostate tissue.
Radiation therapy is the use of high-energy rays to destroy cancer cells. A doctor who specializes in giving radiation therapy to treat cancer is called a radiation oncologist. A radiation therapy regimen, or schedule, usually consists of a specific number of treatments given over a set period of time.
External-beam radiation therapy. External-beam radiation therapy is the most common type of radiation treatment. The radiation oncologist uses a machine located outside the body to focus a beam of x-rays on the area with cancer.
One method of external-beam radiation therapy used to treat prostate cancer is called hypofractionated radiation therapy. This is when a person receives a higher daily dose of radiation therapy given over a shorter period, instead of lower doses given over a longer period. Extreme hypofraction radiation therapy is when the entire treatment is delivered in 5 or fewer treatments. Moderate hypofraction radiation therapy regimens typically include 20 to 28 treatments. This is also called stereotactic body radiation therapy (SBRT) or stereotactic ablative radiation therapy (SABR).
People who receive hypofractionated radiation therapy may have a slightly higher risk of some short-term side effects after treatment compared with those who receive regular external-beam radiation therapy. This may include gastrointestinal side effects.
Brachytherapy. Brachytherapy, or internal radiation therapy, is the insertion of radioactive sources directly into the prostate. These sources, called seeds, give off radiation just around the area where they are inserted and may be left for a short time (high-dose rate) or for a longer time (low-dose rate). Low-dose-rate seeds are left in the prostate permanently and work for up to 1 year after they are inserted. However, how long they work depends on the source of radiation. High-dose-rate brachytherapy is usually left in the body for less than 30 minutes, but it may need to be given more than once.
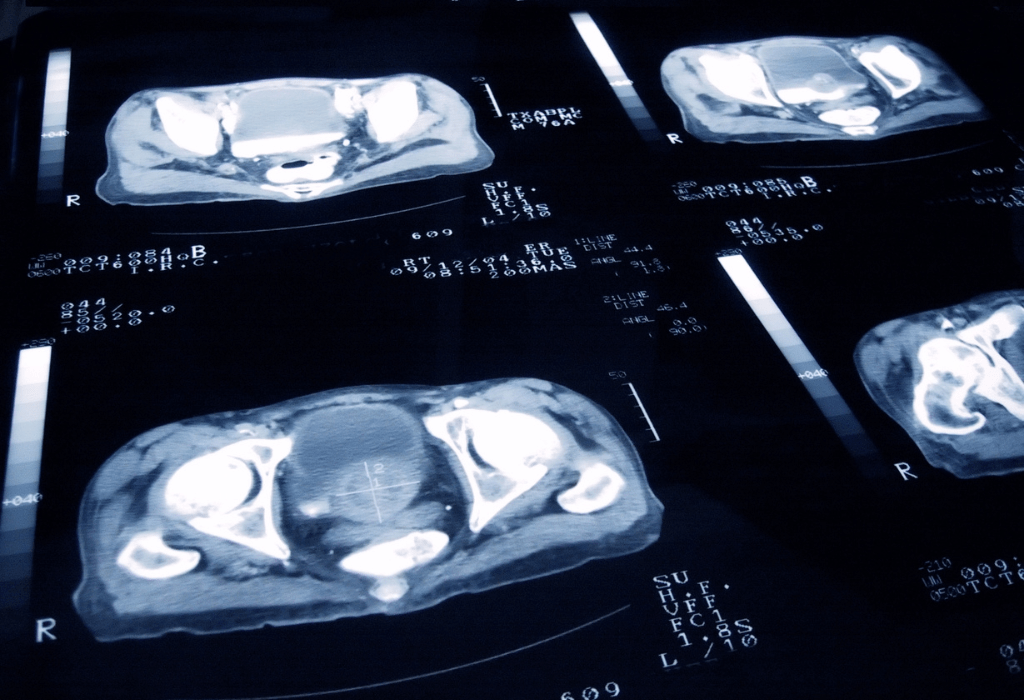
Intensity-modulated radiation therapy (IMRT). IMRT is a type of external-beam radiation therapy that uses CT scans to form a 3D picture of the prostate before treatment. A computer uses this information about the size, shape, and location of the prostate cancer to determine how much radiation is needed to destroy it. With IMRT, high doses of radiation can be directed at the prostate without increasing the risk of damaging nearby organs.
Proton therapy. Proton therapy, also called proton beam therapy, is a type of external-beam radiation therapy that uses protons rather than x-rays. At high energy, protons can destroy cancer cells. Current research has not shown that proton therapy provides any more benefit to people with prostate cancer than traditional radiation therapy. It can also be more expensive.
Treatments using medication are used to destroy cancer cells. Medication may be given through the bloodstream to reach cancer cells throughout the body. When a drug is given this way, it is called systemic therapy.
This type of medication is generally prescribed by a medical oncologist, a doctor who specializes in treating cancer with medication.
Medications are often given through an intravenous (IV) tube placed into a vein using a needle or as a pill or capsule that is swallowed (orally). If you are given oral medications, be sure to ask your health care team about how to safely store and handle it.
The types of medications used for prostate cancer include:
Hormonal therapy
Targeted therapy
Chemotherapy
Immunotherapy
Radiopharmaceuticals
Bone-modifying drugs
Complications of prostate cancer and its treatments include:
Cancer that spreads (metastasizes). Prostate cancer can spread to nearby organs, such as your bladder, or travel through your bloodstream or lymphatic system to your bones or other organs. Prostate cancer that spreads to the bones can cause pain and broken bones. Once prostate cancer has spread to other areas of the body, it may still respond to treatment and may be controlled, but it's unlikely to be cured.
Incontinence. Both prostate cancer and its treatment can cause urinary incontinence. Treatment for incontinence depends on the type you have, how severe it is, and the likelihood it will improve over time. Treatment options may include medications, catheters, and surgery.
Erectile dysfunction. Erectile dysfunction can result from prostate cancer or its treatment, including surgery, radiation, or hormone treatments. Medications, vacuum devices that assist in achieving erection & surgery are available to treat erectile dysfunction.
Screening is recommended if you are a man:
The PSA test and DRE are very important tools. They help to find prostate cancer early, before it spreads. When found early, it can be treated early which helps stop or slow the spread of cancer. This is likely to help some men live longer.
A risk of a PSA test is that it may miss detecting cancer (a "false negative"). Or, the test may be a "false positive," suggesting something is wrong when you are actually healthy. A false positive result may lead to a biopsy that isn't needed. The test might also detect very slow growing cancer that will never cause problems if left untreated
A biopsy is a type of minor surgery. For a prostate biopsy, tiny pieces of tissue are removed from the prostate and looked at under a microscope. The pathologist is the doctor who will look carefully at the tissue samples to look for cancer cells. This is the only way to know for sure if you have prostate cancer.
The decision to have a biopsy is based on PSA and DRE results. Your doctor will also consider your family history of prostate cancer, ethnicity, biopsy history and other health factors.
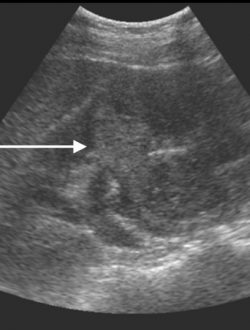
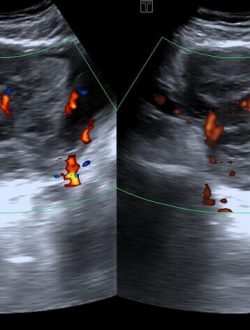
Prostate biopsy is usually done using an ultrasound probe to look at the prostate and guide the biopsy. You may be given an enema and antibiotics to prevent infection. For the test, you will lie on your side as the probe goes into the rectum. First, your provider takes a picture of the prostate using ultrasound. Your healthcare provider will note the prostate gland's size, shape and any abnormalities. He/she will also look for shadows, which might signal cancer. Not all prostate cancers can be seen, and not all shadows are cancer. The prostate gland is then numbed (anesthetized) with a needle passed through the probe. Then, the provider removes very small pieces of your prostate using a biopsy device. The amount of tissue removed depends on the size of the gland, PSA results and past biopsies.








Dr. Utture is Outstanding Doctor who gave good treatment to my 75 years old mother who was suffering from Kidney problem and stomach ache since last 3 years.
Thanks to Dr. Utture
Regards
I have been treated by Dr Anand Utture for multiple kidney stones.He is very knowledgeable, gives right advice, easily approachable and explains in simple language the problem and course of treatment.Takes special care of his patients, truly dedicated doctor
Extremely grateful to Dr Anand Utture for his timely and accurate diagnosis for treating my mother (81 years) for her kidney stones.
very experienced urologist & has done correct diagnosis & treatment of My Grandmother(81 yrs) for kidney stones.
















It’s common for men who have received an abnormal prostate cancer screening—typically discovered through a prostate-specific antigen blood test or digital rectal exam—to be referred to a urologist for further testing. The urologist will conduct a prostate biopsy to determine if cancer cells are present.
Not all growths in the prostate are cancerous, and not all prostate problems indicate cancer. Other conditions that cause similar prostate cancer symptoms include:
Benign prostatic hyperplasia (BPH): At some point, almost every man will develop benign prostatic hyperplasia (BPH). This condition enlarges the prostate gland but doesn’t increase cancer risk. The swollen gland squeezes the urethra and blocks the flow of semen and urine. Medications, and sometimes surgery, can help.
Prostatitis: Men younger than 50 are more prone to prostatitis, inflammation and swelling of the prostate gland. Bacterial infections are often the cause. Treatments include antibiotics or other medications.
PSA blood levels can fluctuate for many reasons – even in the same man over time – so there is no specific level or range that is considered to be “normal.” For instance, some factors that can affect the level of PSA in the blood include:
In general, however, the likelihood of prostate cancer increases along with blood PSA levels. If a relatively high PSA level (approximately 4.0 ng/mL or above) is detected, most physicians recommend repeat testing supplemented by other noninvasive tests, such as an MRI scan, rather than immediately ordering a biopsy.
Some possible risks of a radical prostatectomy include:
With regard to prostate cancer, many patients receive their diagnosis from a urologist. If a urologist suspects prostate cancer after performing a physical examination and a digital rectal examination (DRE) and/or a prostate-specific antigen test (PSA), he or she will likely perform a prostate biopsy and order additional imaging tests.
If prostate cancer is present, the urologist will generally assign a Gleason score, which indicates how likely the cancer is to metastasize, or spread. In cases where surgery is necessary to remove cancerous tissue, the urologist may perform a procedure such as a laparoscopic radical prostatectomy. Other aspects of prostate cancer treatment are handled by specialists in other fields, such as oncology and radiology.
of a routine physical examination, it’s important to regularly visit your medical provider for checkups.
Dr Anand Utture is a Senior Urologist who is internationally recognized for his surgical expertise and academic contribution to the field of Urology.
Book AppointmentMake an appointment with your doctor if you have any signs and symptoms that worry you.
Seek immediate medical attention if you experience: